Adrenergic Receptors
Understanding Adrenergic Receptors and Vasoactive Drugs in the NICU
If you’ve ever started a vasoactive drip at 3 a.m. and felt your brain juggling “alpha, beta, and dopamine receptors” all at once — you’re not alone. These drugs can feel intimidating because their effects change depending on which receptors they act on and at what dose. But once you understand the why behind each receptor, everything clicks into place.
Let’s break it down together:
Inotropes vs. Vasopressors: What’s the Difference?
Before diving into the pharmacology, it helps to separate two key terms that often get used interchangeably but mean very different things.
Vasopressors cause vasoconstriction — they tighten the vessels, increasing systemic vascular resistance (SVR) and therefore raising blood pressure.
Inotropes increase cardiac contractility (the strength of each heartbeat). This boosts cardiac output, helping improve tissue perfusion.
Some medications do both, which is why we often call them inotropic–vasoactive agents. Others also have lusitropic properties (improving myocardial relaxation during diastole) or chronotropic effects (increasing heart rate).
In the NICU, we rarely think about these drugs in isolation — instead, we look at which receptors they target and what the baby’s cardiovascular physiology needs in that moment.
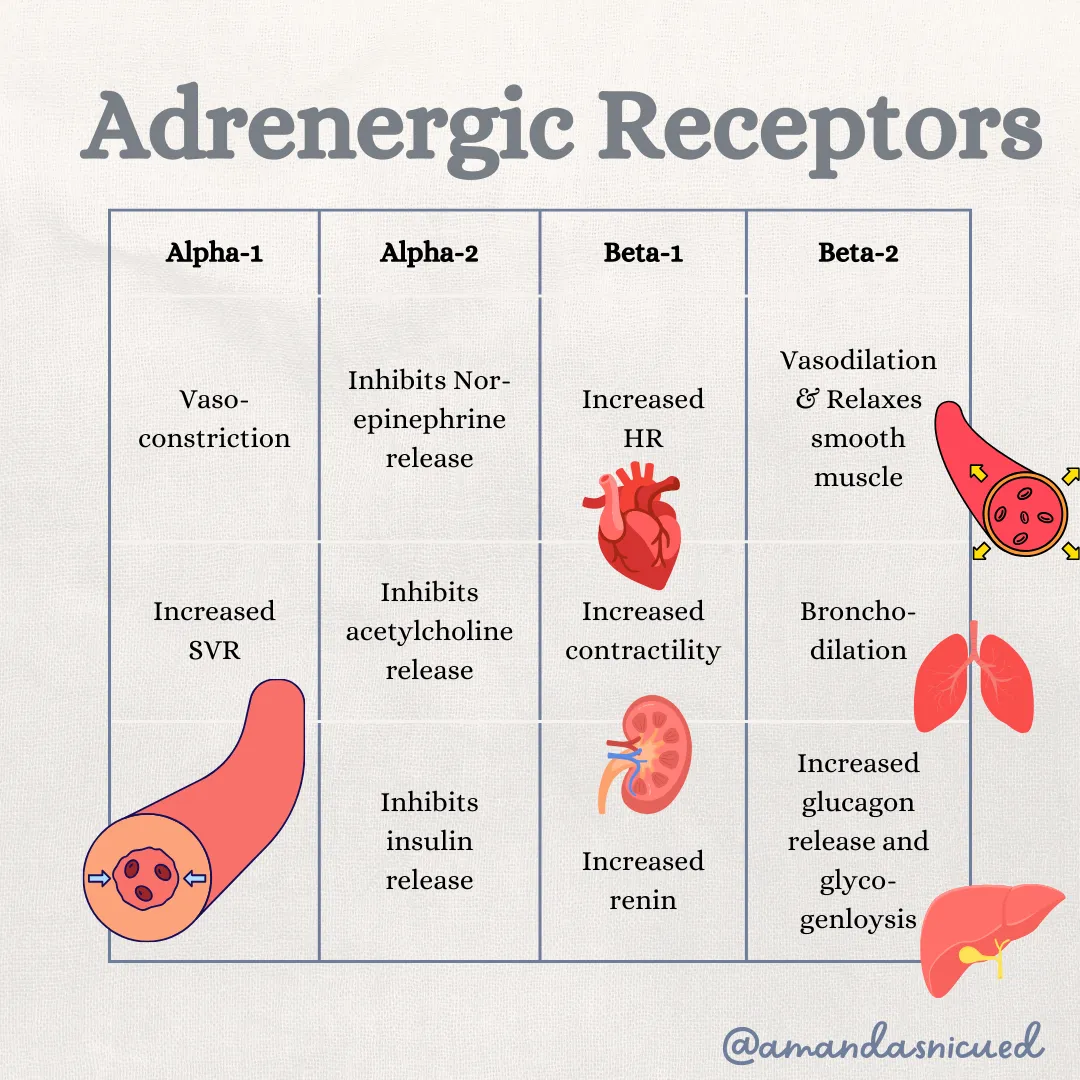
Why Adrenergic Receptors Matter
Adrenergic receptors sit on cell surfaces throughout the body and respond to catecholamines like epinephrine, norepinephrine, and dopamine. When activated, they regulate the sympathetic nervous system — the body’s built-in “fight-or-flight” response.
Understanding which receptor is being activated helps predict a drug’s effect. Here’s a quick roadmap:
Dopaminergic Receptors (D₁ and D₂)
At low doses, dopamine acts on D₁ and D₂ receptors, increasing renal and mesenteric blood flow.
That’s where the old concept of “renal-dose dopamine” came from — giving a low infusion rate to “help the kidneys.”
However, studies have shown this benefit is limited and only effective if perfusion and intravascular volume are already adequate. In shock states, dopamine’s dose often escalates beyond the dopaminergic range, where it begins acting on alpha and beta receptors instead — changing its effects entirely.

Alpha-1 Receptors
Alpha-1 stimulation causes vasoconstriction. When vessels tighten, SVR rises and diastolic pressure increases.
So when do we want this?
When the baby’s vessels are overly dilated — for example, in septic shock or during anesthesia-induced vasodilation. Drugs with strong alpha-1 activity help restore tone and perfusion pressure.
Alpha-2 Receptors
Alpha-2 is more of a feedback control receptor. When activated, it reduces norepinephrine release and dampens sympathetic outflow.
Clinically, we don’t rely on alpha-2 for hemodynamic management in neonates, but it explains the sedative and stress-modulating effects of medications like clonidine or dexmedetomidine. These drugs are often used for comfort, sedation, or reducing agitation in critically ill infants — not primarily for blood pressure control, but through this same receptor system.
Beta-1 Receptors
Think heart when you hear beta-1.
Stimulation increases:
Heart rate (positive chronotropy)
Contractility (positive inotropy)
That means beta-1 agonists are especially useful when we need to improve cardiac output, such as in cardiogenic shock, post-asphyxia myocardial dysfunction, or low-output states after surgery.
Beta-2 Receptors
Beta-2 affects lungs and vascular smooth muscle.
Activation leads to bronchodilation and vasodilation — helpful in airway disease, but sometimes tricky in shock.
In the NICU, this becomes particularly relevant when we use medications like dobutamine or epinephrine. Both stimulate beta-1 and beta-2 receptors, but the balance between the two determines the net clinical effect:
More beta-1 → increased contractility and heart rate
More beta-2 → vasodilation and potential drop in blood pressure
So, dose and context matter tremendously.
💡 Pro Tip: Instead of memorizing which drug “does what,” start by asking which receptor do I want to target? Then choose the medication and dose that fits the baby’s physiology.
Bringing It All Together
Each vasoactive or inotropic drug we use in the NICU — dopamine, dobutamine, epinephrine, norepinephrine, milrinone — acts on a unique combination of these receptors. Understanding that mix helps you anticipate what will happen next:
Rising BP but worsening perfusion? Too much alpha-1.
Improved contractility but tachycardia? Predominant beta-1 effect.
Falling BP with bronchodilation? Likely a strong beta-2 response.
And when you understand why that’s happening, you can titrate confidently and communicate effectively with your team.
Final Thoughts
Adrenergic receptors may sound like alphabet soup at first, but they’re the foundation of understanding how vasoactive and inotropic drugs work. Once you see the connections between receptor, dose, and physiologic effect, these medications stop feeling intimidating — and start feeling like a science you can master.
Your next patient on dopamine, dobutamine, or epinephrine isn’t just a number on a pump — they’re a window into applied physiology.
📘 Ready to go deeper?
Join hundreds of NICU nurses in my Neonatal Certification Review Course — designed to simplify complex topics like this and help you pass your RNC-NIC or CCRN-N exam with confidence.
Click here to learn more and enroll today!
References
Gardner, S. L., Carter, B. S., Enzman-Hines, M. I., & Hernandez, J. A. (2021). Handbook of Neonatal Intensive Care: An Interprofessional Approach (9th ed.). Elsevier.
Martin, R. J., Fanaroff, A. A., & Walsh, M. C. (2020). Fanaroff and Martin’s Neonatal-Perinatal Medicine: Diseases of the Fetus and Infant (11th ed.). Elsevier.
Verklan, M. T., & Walden, M. (2021). Core Curriculum for Neonatal Intensive Care Nursing (6th ed.). Elsevier.
