Amanda's NICU ED Blogs
RECENT BLOG ARTICLES

Modes of Ventilation in the NICU

Modes of Ventilation in the NICU
In the neonatal intensive care unit (NICU), respiratory support plays a crucial role in managing the respiratory distress of fragile infants. Understanding the different modes of ventilation is essential for NICU nurses to provide optimal care. In this discussion, we will explore both invasive and non-invasive ventilation modes that are commonly used in the NICU. By familiarizing ourselves with these modes, we can enhance our knowledge and skills to effectively support newborns requiring respiratory assistance.
I. Invasive Ventilation:
Invasive ventilation involves the use of endotracheal intubation and a mechanical ventilator. The following modes are commonly seen in the NICU:
1. High-Frequency Oscillatory Ventilation (HFOV):
HFOV delivers small, rapid breaths at superimposed high-frequency oscillations. It is used in cases of severe respiratory failure or when conventional ventilation fails to provide adequate gas exchange. HFOV provides lung recruitment and optimization of oxygenation while minimizing the risk of lung injury. HFOV provides active inhalation and exhalation at a very fast rate.
2. High-Frequency Jet Ventilation (HFJV):
HFJV utilizes small, rapid bursts of gas with very low tidal volumes through a jet catheter. It is particularly useful for infants with air leak syndromes, as it allows for effective ventilation with low mean airway pressures. HFJV can help maintain lung recruitment and gas exchange in critically ill neonates. HFJV provides an active inhalation and a passive exhalation.
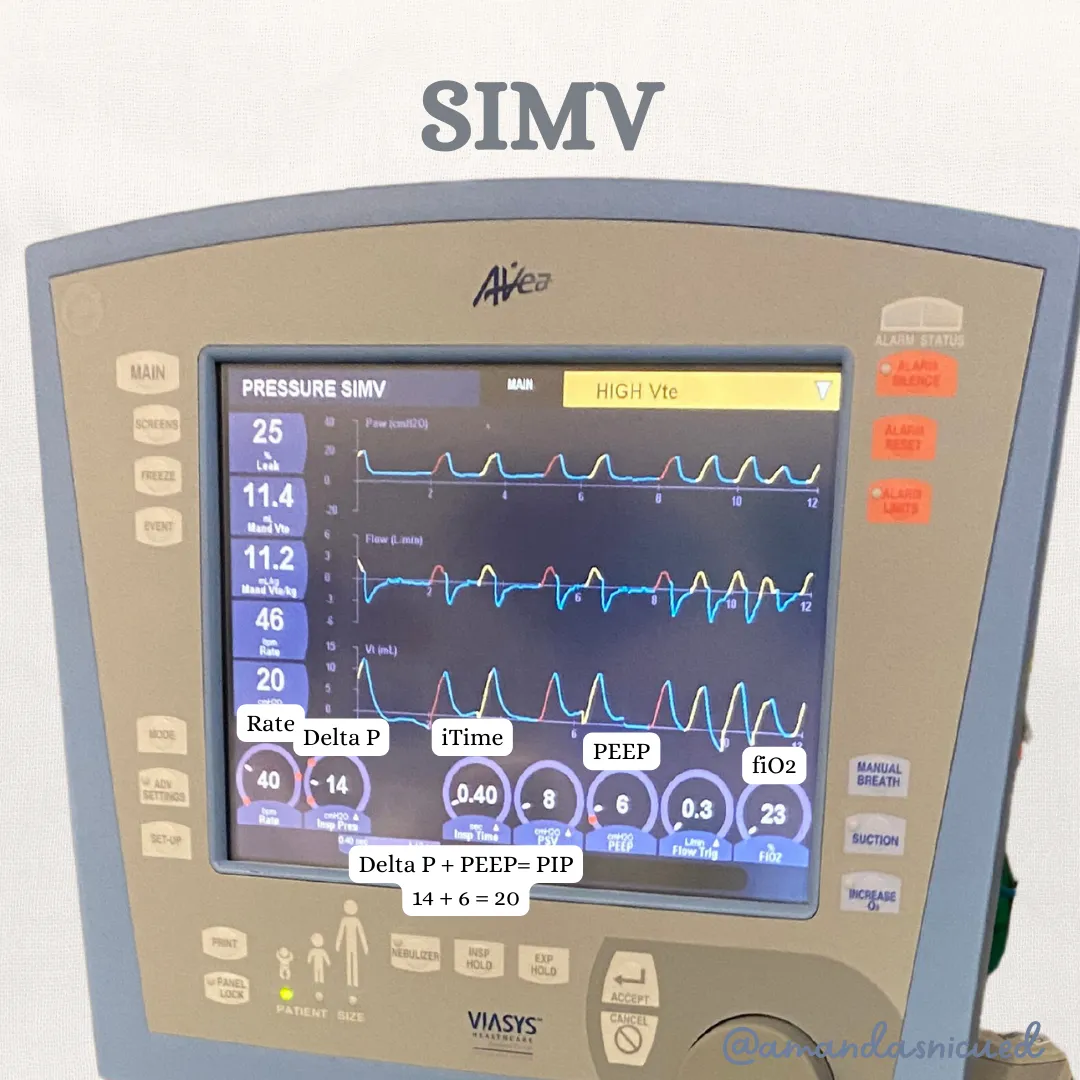
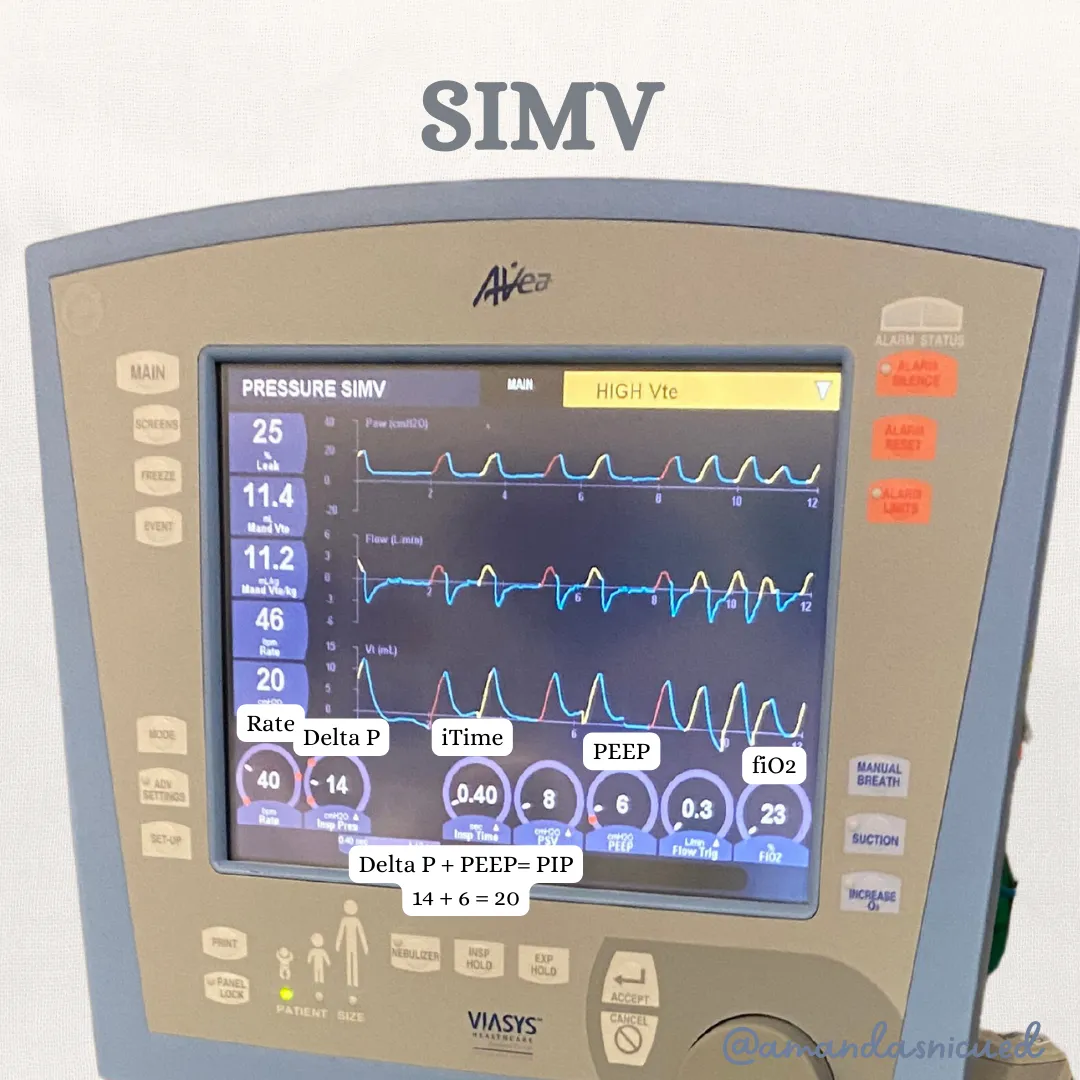
3. Synchronized Intermittent Mandatory Ventilation (SIMV):
SIMV delivers a preset number of mandatory breaths per minute, synchronized with the infant's spontaneous breaths. It allows the baby to have some control over their respiratory efforts while receiving support. SIMV is often used during weaning from mechanical ventilation, gradually decreasing the support provided.
4. Assist-Control Ventilation (A/C):
A/C ventilation delivers a predetermined number of mandatory breaths, but unlike SIMV, it does not synchronize with the infant's spontaneous breaths. With A/C ventilation, each breath is fully supported by the ventilator. It is commonly used in situations where the infant requires full respiratory support.
II. Non-Invasive Ventilation:
Non-invasive ventilation provides respiratory support without the need for endotracheal intubation. The following modes are frequently utilized in the NICU:
1. Nasal Intermittent Positive Pressure Ventilation (NIPPV):
NIPPV delivers positive pressure breaths via nasal prongs or a nasal mask. It helps improve oxygenation and ventilation without an endotracheal tube. NIPPV is commonly used as a transition from invasive ventilation or as initial respiratory support for infants who do not require intubation.
2. Nasal Continuous Positive Airway Pressure (NCPAP):
NCPAP delivers a constant positive pressure throughout the respiratory cycle via nasal prongs or a nasal mask. It helps maintain lung recruitment, reduce work of breathing, and improve oxygenation. NCPAP is widely used for respiratory support in preterm infants with respiratory distress syndrome (RDS) or other respiratory conditions.
3. High Flow Nasal Cannula (HFNC):
HFNC delivers humidified and heated oxygen at a high flow rate through nasal prongs. It provides a comfortable and well-tolerated form of respiratory support, improving oxygenation and reducing respiratory effort. HFNC is effective in managing mild to moderate respiratory distress and is increasingly used as an alternative to NCPAP.
4. Low Flow Nasal Cannula:
Low Flow Nasal Cannula delivers oxygen at a low flow rate through nasal prongs. While not a ventilation mode per se, it is worth mentioning as it is commonly used to deliver supplemental oxygen to stable infants who require minimal respiratory support.
Conclusion
Understanding the various modes of ventilation in the NICU is essential for NICU nurses. By familiarizing ourselves with both invasive and non-invasive ventilation modes, we can tailor respiratory support to the specific needs of each newborn. Collaboration between healthcare providers, ongoing assessment, and vigilant monitoring are key to optimizing respiratory care and promoting positive outcomes for these fragile infants.
Reference:
Kieran EA, Walsh MC. Noninvasive and invasive respiratory support. In: Cloherty JP, Eichenwald EC, Stark AR, eds. Manual of Neonatal Care. 8th ed. Philadelphia, PA: Wolters Kluwer; 2020:226-257.
Lampland AL, Plumm B, Meyers PA, Worwa CT, Mammel MC. Noninvasive pressure support ventilation in the preterm neonate: reducing endotracheal intubation, bronchopulmonary dysplasia, and ventilator-associated pneumonia. J Perinatol. 2017;37(11):1250-1255. doi:10.1038/jp.2017.117
Respiratory and Blood Gas Blogs
Modes of Ventilation in the NICU

Modes of Ventilation in the NICU
In the neonatal intensive care unit (NICU), respiratory support plays a crucial role in managing the respiratory distress of fragile infants. Understanding the different modes of ventilation is essential for NICU nurses to provide optimal care. In this discussion, we will explore both invasive and non-invasive ventilation modes that are commonly used in the NICU. By familiarizing ourselves with these modes, we can enhance our knowledge and skills to effectively support newborns requiring respiratory assistance.
I. Invasive Ventilation:
Invasive ventilation involves the use of endotracheal intubation and a mechanical ventilator. The following modes are commonly seen in the NICU:
1. High-Frequency Oscillatory Ventilation (HFOV):
HFOV delivers small, rapid breaths at superimposed high-frequency oscillations. It is used in cases of severe respiratory failure or when conventional ventilation fails to provide adequate gas exchange. HFOV provides lung recruitment and optimization of oxygenation while minimizing the risk of lung injury. HFOV provides active inhalation and exhalation at a very fast rate.
2. High-Frequency Jet Ventilation (HFJV):
HFJV utilizes small, rapid bursts of gas with very low tidal volumes through a jet catheter. It is particularly useful for infants with air leak syndromes, as it allows for effective ventilation with low mean airway pressures. HFJV can help maintain lung recruitment and gas exchange in critically ill neonates. HFJV provides an active inhalation and a passive exhalation.
3. Synchronized Intermittent Mandatory Ventilation (SIMV):
SIMV delivers a preset number of mandatory breaths per minute, synchronized with the infant's spontaneous breaths. It allows the baby to have some control over their respiratory efforts while receiving support. SIMV is often used during weaning from mechanical ventilation, gradually decreasing the support provided.
4. Assist-Control Ventilation (A/C):
A/C ventilation delivers a predetermined number of mandatory breaths, but unlike SIMV, it does not synchronize with the infant's spontaneous breaths. With A/C ventilation, each breath is fully supported by the ventilator. It is commonly used in situations where the infant requires full respiratory support.
II. Non-Invasive Ventilation:
Non-invasive ventilation provides respiratory support without the need for endotracheal intubation. The following modes are frequently utilized in the NICU:
1. Nasal Intermittent Positive Pressure Ventilation (NIPPV):
NIPPV delivers positive pressure breaths via nasal prongs or a nasal mask. It helps improve oxygenation and ventilation without an endotracheal tube. NIPPV is commonly used as a transition from invasive ventilation or as initial respiratory support for infants who do not require intubation.
2. Nasal Continuous Positive Airway Pressure (NCPAP):
NCPAP delivers a constant positive pressure throughout the respiratory cycle via nasal prongs or a nasal mask. It helps maintain lung recruitment, reduce work of breathing, and improve oxygenation. NCPAP is widely used for respiratory support in preterm infants with respiratory distress syndrome (RDS) or other respiratory conditions.
3. High Flow Nasal Cannula (HFNC):
HFNC delivers humidified and heated oxygen at a high flow rate through nasal prongs. It provides a comfortable and well-tolerated form of respiratory support, improving oxygenation and reducing respiratory effort. HFNC is effective in managing mild to moderate respiratory distress and is increasingly used as an alternative to NCPAP.
4. Low Flow Nasal Cannula:
Low Flow Nasal Cannula delivers oxygen at a low flow rate through nasal prongs. While not a ventilation mode per se, it is worth mentioning as it is commonly used to deliver supplemental oxygen to stable infants who require minimal respiratory support.
Conclusion
Understanding the various modes of ventilation in the NICU is essential for NICU nurses. By familiarizing ourselves with both invasive and non-invasive ventilation modes, we can tailor respiratory support to the specific needs of each newborn. Collaboration between healthcare providers, ongoing assessment, and vigilant monitoring are key to optimizing respiratory care and promoting positive outcomes for these fragile infants.
Reference:
Kieran EA, Walsh MC. Noninvasive and invasive respiratory support. In: Cloherty JP, Eichenwald EC, Stark AR, eds. Manual of Neonatal Care. 8th ed. Philadelphia, PA: Wolters Kluwer; 2020:226-257.
Lampland AL, Plumm B, Meyers PA, Worwa CT, Mammel MC. Noninvasive pressure support ventilation in the preterm neonate: reducing endotracheal intubation, bronchopulmonary dysplasia, and ventilator-associated pneumonia. J Perinatol. 2017;37(11):1250-1255. doi:10.1038/jp.2017.117
Cardiac Blogs
Modes of Ventilation in the NICU

Modes of Ventilation in the NICU
In the neonatal intensive care unit (NICU), respiratory support plays a crucial role in managing the respiratory distress of fragile infants. Understanding the different modes of ventilation is essential for NICU nurses to provide optimal care. In this discussion, we will explore both invasive and non-invasive ventilation modes that are commonly used in the NICU. By familiarizing ourselves with these modes, we can enhance our knowledge and skills to effectively support newborns requiring respiratory assistance.
I. Invasive Ventilation:
Invasive ventilation involves the use of endotracheal intubation and a mechanical ventilator. The following modes are commonly seen in the NICU:
1. High-Frequency Oscillatory Ventilation (HFOV):
HFOV delivers small, rapid breaths at superimposed high-frequency oscillations. It is used in cases of severe respiratory failure or when conventional ventilation fails to provide adequate gas exchange. HFOV provides lung recruitment and optimization of oxygenation while minimizing the risk of lung injury. HFOV provides active inhalation and exhalation at a very fast rate.
2. High-Frequency Jet Ventilation (HFJV):
HFJV utilizes small, rapid bursts of gas with very low tidal volumes through a jet catheter. It is particularly useful for infants with air leak syndromes, as it allows for effective ventilation with low mean airway pressures. HFJV can help maintain lung recruitment and gas exchange in critically ill neonates. HFJV provides an active inhalation and a passive exhalation.
3. Synchronized Intermittent Mandatory Ventilation (SIMV):
SIMV delivers a preset number of mandatory breaths per minute, synchronized with the infant's spontaneous breaths. It allows the baby to have some control over their respiratory efforts while receiving support. SIMV is often used during weaning from mechanical ventilation, gradually decreasing the support provided.
4. Assist-Control Ventilation (A/C):
A/C ventilation delivers a predetermined number of mandatory breaths, but unlike SIMV, it does not synchronize with the infant's spontaneous breaths. With A/C ventilation, each breath is fully supported by the ventilator. It is commonly used in situations where the infant requires full respiratory support.
II. Non-Invasive Ventilation:
Non-invasive ventilation provides respiratory support without the need for endotracheal intubation. The following modes are frequently utilized in the NICU:
1. Nasal Intermittent Positive Pressure Ventilation (NIPPV):
NIPPV delivers positive pressure breaths via nasal prongs or a nasal mask. It helps improve oxygenation and ventilation without an endotracheal tube. NIPPV is commonly used as a transition from invasive ventilation or as initial respiratory support for infants who do not require intubation.
2. Nasal Continuous Positive Airway Pressure (NCPAP):
NCPAP delivers a constant positive pressure throughout the respiratory cycle via nasal prongs or a nasal mask. It helps maintain lung recruitment, reduce work of breathing, and improve oxygenation. NCPAP is widely used for respiratory support in preterm infants with respiratory distress syndrome (RDS) or other respiratory conditions.
3. High Flow Nasal Cannula (HFNC):
HFNC delivers humidified and heated oxygen at a high flow rate through nasal prongs. It provides a comfortable and well-tolerated form of respiratory support, improving oxygenation and reducing respiratory effort. HFNC is effective in managing mild to moderate respiratory distress and is increasingly used as an alternative to NCPAP.
4. Low Flow Nasal Cannula:
Low Flow Nasal Cannula delivers oxygen at a low flow rate through nasal prongs. While not a ventilation mode per se, it is worth mentioning as it is commonly used to deliver supplemental oxygen to stable infants who require minimal respiratory support.
Conclusion
Understanding the various modes of ventilation in the NICU is essential for NICU nurses. By familiarizing ourselves with both invasive and non-invasive ventilation modes, we can tailor respiratory support to the specific needs of each newborn. Collaboration between healthcare providers, ongoing assessment, and vigilant monitoring are key to optimizing respiratory care and promoting positive outcomes for these fragile infants.
Reference:
Kieran EA, Walsh MC. Noninvasive and invasive respiratory support. In: Cloherty JP, Eichenwald EC, Stark AR, eds. Manual of Neonatal Care. 8th ed. Philadelphia, PA: Wolters Kluwer; 2020:226-257.
Lampland AL, Plumm B, Meyers PA, Worwa CT, Mammel MC. Noninvasive pressure support ventilation in the preterm neonate: reducing endotracheal intubation, bronchopulmonary dysplasia, and ventilator-associated pneumonia. J Perinatol. 2017;37(11):1250-1255. doi:10.1038/jp.2017.117
hey nurses don't miss out
© Copyright 2024. AmandasNICUEd. All rights reserved. | Terms & Conditions | Privacy Policy Contact: [email protected]
