Amanda's NICU ED Blogs
RECENT BLOG ARTICLES

Neonatal Head to Toe Assessment
Hi there,
I just returned from an amazing conference down in San Diego. I always love learning from the experts about the latest research, QI projects, and ideas to better care for our patients. Do you attend conferences? I think it's a great way to continue developing professionally, staying curious, and learning how we can provide better care for our babies. Let me know if you are planning on attending any upcoming neonatal conferences, maybe I'll see you there!
Neonatal Head-to-Toe Assessment: A Guide for NICU Nurses
When you first hold a newborn patient in your hands as a NICU nurse, every tiny detail matters. Performing a comprehensive neonatal assessment isn't just a clinical task—it's your window into understanding what your patient needs when they can't tell you themselves. This structured approach blends careful observation, precise auscultation, and gentle palpation to reveal crucial clinical information that could make all the difference in a newborn's care journey.

The Art of Silent Assessment: Observation First 👀
Before your hands ever touch the baby, your eyes should be collecting vital information. This initial observation period tells a story:
Watch how the newborn's skin tone appears across their body—is it the healthy pink we hope to see, or are you noticing concerning pallor, plethora, jaundice, or the bluish tint of cyanosis? Notice how the baby moves—are their movements smooth and purposeful, or do you see concerning limpness or jitteriness that suggest neurological or musculoskeletal issues? Pay special attention to their breathing effort—the subtle signs of retractions between the ribs, nostrils flaring with each breath, or the telltale grunting of respiratory distress can alert you to problems before monitors do. Finally, assess their state of alertness—whether peacefully sleeping, quietly observing the world, actively engaged, or crying in distress—as this offers insights into both their neurological status and immediate needs.
Head Assessment 👶
The newborn's head holds many clues about their birth experience and neurological health:
When you palpate the fontanelles and suture lines, you're checking not just for normal development but for signs of increased intracranial pressure or premature fusion. You'll likely encounter common findings like caput succedaneum (swelling that crosses suture lines and typically resolves within days) or cephalohematoma (swelling confined by suture lines and potentially taking weeks to resolve). But remain vigilant for the rare but dangerous subgaleal hemorrhage—a mobile, boggy scalp mass that can rapidly lead to hypovolemic shock and requires immediate intervention.
Skin Assessment 🖐️
A newborn's skin can tell us a lot about their overall health, don't forget the skin is our bodies largest organ:
The creamy vernix protecting a term newborn's skin and the fine lanugo covering a premature baby's body are normal findings that tell you about gestational age. You'll commonly spot benign conditions like erythema toxicum (those harmless white vesicles on red bases that are sometimes referred to as “baby acne”) or tiny white milia cysts across the nose and cheeks. While many birthmarks like Mongolian spots or strawberry hemangiomas are harmless, be alert for concerning signs like petechiae, pustules, or large bruises that might signal infection or bleeding disorders requiring prompt attention.
Cardiovascular System 🫀
The cardiovascular assessment goes far beyond just checking numbers on the monitor:
You should auscultate a heart rate between 100-160 beats per minute in a calm, resting newborn. Listen carefully through all cardiac cycles for murmurs that might suggest structural heart problems. The comparison between brachial and femoral pulses is particularly crucial—diminished or absent femoral pulses could be your first clue of coarctation of the aorta, a condition requiring timely intervention. And don't forget signs of perfusion, like capillary refill... we want to see a brisk refill under 3 seconds.
Respiratory Assessment 🫁
A newborn's breathing pattern reveals volumes about their adaptation to extrauterine life:
While counting those 40-60 breaths per minute, you're watching for the subtle signs of respiratory distress that might indicate the need for support. The fine crackles you hear during the first few hours are often simply the sound of fetal lung fluid clearing—a normal transition phenomenon. However, high-pitched stridor demands attention as it suggests airway obstruction. And if your stethoscope picks up bowel sounds where lung sounds should be, consider the possibility of congenital diaphragmatic hernia (CDH), where abdominal organs have migrated into the chest cavity.‼️
Abdominal Assessment 🍼
The abdomen holds clues about multiple organ systems:
A symmetrical, gently rounded abdomen is what we hope to find, but deviations tell important stories. A scaphoid (sunken) abdomen in conjunction with respiratory distress might suggest CDH, while distention could indicate anything from harmless "CPAP belly" to a concerning intestinal obstruction. Those active bowel sounds should appear within the first hours after birth as the intestines fill with gas.
Genitourinary Assessment 💩
This assessment provides insights about both current function and future development:
For male infants, checking for hypospadias isn't just about noting abnormal urethral placement—it's also critical information for preventing inappropriate circumcision that could complicate future surgical repair. In female infants, the pseudo-menses you might observe is simply the body's response to maternal hormones withdrawal—a normal finding that often alarms new parents. Tracking urinary output in the precise measurements in mL/kg/hr gives you quantifiable data about kidney function and overall fluid balance that guides critical treatment decisions.
Musculoskeletal & Neurological Assessment 🧠
How a newborn moves and responds reveals their neurological integrity:
When you check the clavicles after a difficult delivery, you're looking for the subtle signs of fracture that might explain decreased arm movement. The primitive reflexes—Moro, grasp, stepping, Babinski, Galant..—provide a window into neurological development and function. An asymmetric Moro reflex might be your first indication of brachial plexus injury, while asymmetric gluteal folds could signal developmental dysplasia of the hip that, if caught early, can prevent years of mobility challenges.
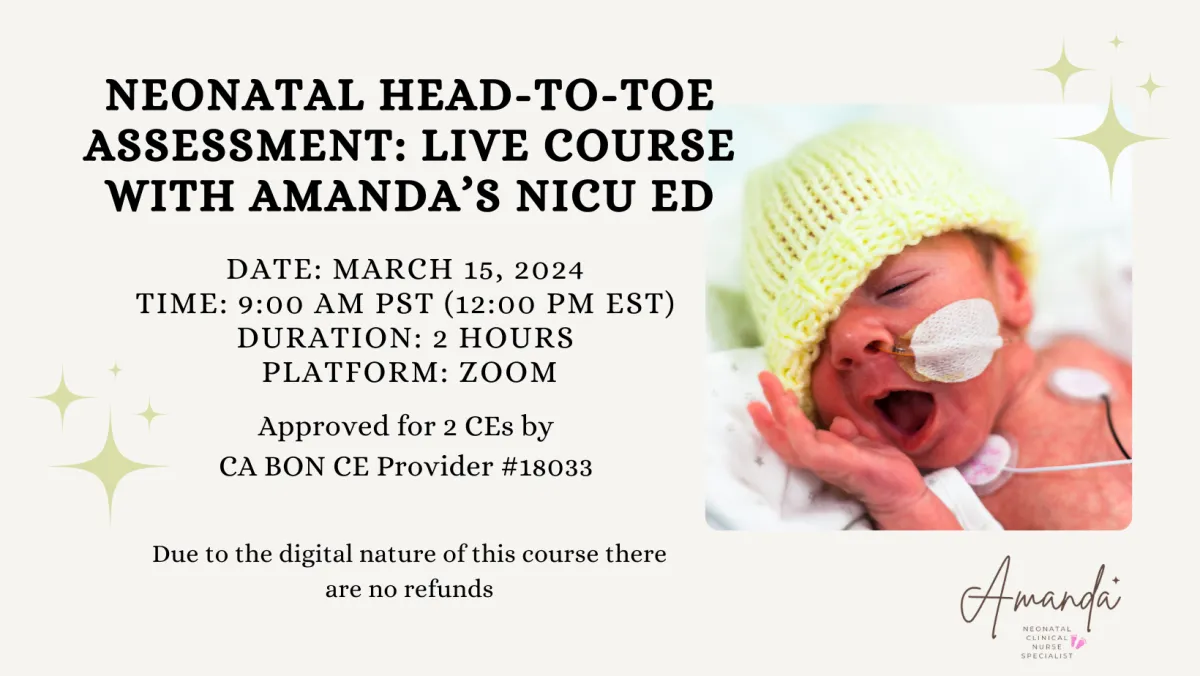
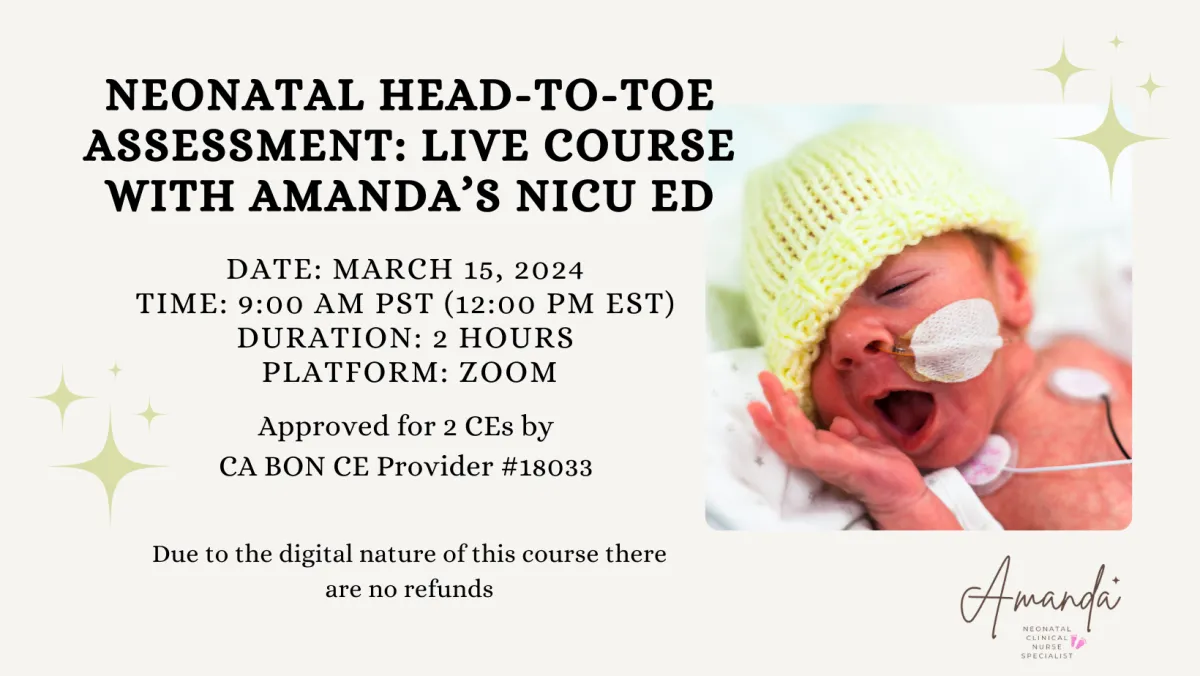
Transform Your Assessment Skills: Join Me on March 15! 🤓
Imagine moving beyond textbook knowledge to confident, clinical expertise in neonatal assessment. That's exactly what my live course on March 15 offers!
Whether you're new to the NICU or looking to refine your skills, this interactive session will transform how you approach each neonatal patient—giving you practical techniques and a supportive community of passionate nurses, all focused on mastering neonatal assessment.
📌 Reserve your spot now!
✨ Can't make it live or missed the session? No worries! You'll still have access to the recording.
I look forward to helping you develop the confident, nuanced assessment skills that make exceptional NICU nurses. See you there! 💙👶🏽

Wishing you the best
Amanda 💜
Respiratory and Blood Gas Blogs
Neonatal Head to Toe Assessment
Hi there,
I just returned from an amazing conference down in San Diego. I always love learning from the experts about the latest research, QI projects, and ideas to better care for our patients. Do you attend conferences? I think it's a great way to continue developing professionally, staying curious, and learning how we can provide better care for our babies. Let me know if you are planning on attending any upcoming neonatal conferences, maybe I'll see you there!
Neonatal Head-to-Toe Assessment: A Guide for NICU Nurses
When you first hold a newborn patient in your hands as a NICU nurse, every tiny detail matters. Performing a comprehensive neonatal assessment isn't just a clinical task—it's your window into understanding what your patient needs when they can't tell you themselves. This structured approach blends careful observation, precise auscultation, and gentle palpation to reveal crucial clinical information that could make all the difference in a newborn's care journey.

The Art of Silent Assessment: Observation First 👀
Before your hands ever touch the baby, your eyes should be collecting vital information. This initial observation period tells a story:
Watch how the newborn's skin tone appears across their body—is it the healthy pink we hope to see, or are you noticing concerning pallor, plethora, jaundice, or the bluish tint of cyanosis? Notice how the baby moves—are their movements smooth and purposeful, or do you see concerning limpness or jitteriness that suggest neurological or musculoskeletal issues? Pay special attention to their breathing effort—the subtle signs of retractions between the ribs, nostrils flaring with each breath, or the telltale grunting of respiratory distress can alert you to problems before monitors do. Finally, assess their state of alertness—whether peacefully sleeping, quietly observing the world, actively engaged, or crying in distress—as this offers insights into both their neurological status and immediate needs.
Head Assessment 👶
The newborn's head holds many clues about their birth experience and neurological health:
When you palpate the fontanelles and suture lines, you're checking not just for normal development but for signs of increased intracranial pressure or premature fusion. You'll likely encounter common findings like caput succedaneum (swelling that crosses suture lines and typically resolves within days) or cephalohematoma (swelling confined by suture lines and potentially taking weeks to resolve). But remain vigilant for the rare but dangerous subgaleal hemorrhage—a mobile, boggy scalp mass that can rapidly lead to hypovolemic shock and requires immediate intervention.
Skin Assessment 🖐️
A newborn's skin can tell us a lot about their overall health, don't forget the skin is our bodies largest organ:
The creamy vernix protecting a term newborn's skin and the fine lanugo covering a premature baby's body are normal findings that tell you about gestational age. You'll commonly spot benign conditions like erythema toxicum (those harmless white vesicles on red bases that are sometimes referred to as “baby acne”) or tiny white milia cysts across the nose and cheeks. While many birthmarks like Mongolian spots or strawberry hemangiomas are harmless, be alert for concerning signs like petechiae, pustules, or large bruises that might signal infection or bleeding disorders requiring prompt attention.
Cardiovascular System 🫀
The cardiovascular assessment goes far beyond just checking numbers on the monitor:
You should auscultate a heart rate between 100-160 beats per minute in a calm, resting newborn. Listen carefully through all cardiac cycles for murmurs that might suggest structural heart problems. The comparison between brachial and femoral pulses is particularly crucial—diminished or absent femoral pulses could be your first clue of coarctation of the aorta, a condition requiring timely intervention. And don't forget signs of perfusion, like capillary refill... we want to see a brisk refill under 3 seconds.
Respiratory Assessment 🫁
A newborn's breathing pattern reveals volumes about their adaptation to extrauterine life:
While counting those 40-60 breaths per minute, you're watching for the subtle signs of respiratory distress that might indicate the need for support. The fine crackles you hear during the first few hours are often simply the sound of fetal lung fluid clearing—a normal transition phenomenon. However, high-pitched stridor demands attention as it suggests airway obstruction. And if your stethoscope picks up bowel sounds where lung sounds should be, consider the possibility of congenital diaphragmatic hernia (CDH), where abdominal organs have migrated into the chest cavity.‼️
Abdominal Assessment 🍼
The abdomen holds clues about multiple organ systems:
A symmetrical, gently rounded abdomen is what we hope to find, but deviations tell important stories. A scaphoid (sunken) abdomen in conjunction with respiratory distress might suggest CDH, while distention could indicate anything from harmless "CPAP belly" to a concerning intestinal obstruction. Those active bowel sounds should appear within the first hours after birth as the intestines fill with gas.
Genitourinary Assessment 💩
This assessment provides insights about both current function and future development:
For male infants, checking for hypospadias isn't just about noting abnormal urethral placement—it's also critical information for preventing inappropriate circumcision that could complicate future surgical repair. In female infants, the pseudo-menses you might observe is simply the body's response to maternal hormones withdrawal—a normal finding that often alarms new parents. Tracking urinary output in the precise measurements in mL/kg/hr gives you quantifiable data about kidney function and overall fluid balance that guides critical treatment decisions.
Musculoskeletal & Neurological Assessment 🧠
How a newborn moves and responds reveals their neurological integrity:
When you check the clavicles after a difficult delivery, you're looking for the subtle signs of fracture that might explain decreased arm movement. The primitive reflexes—Moro, grasp, stepping, Babinski, Galant..—provide a window into neurological development and function. An asymmetric Moro reflex might be your first indication of brachial plexus injury, while asymmetric gluteal folds could signal developmental dysplasia of the hip that, if caught early, can prevent years of mobility challenges.
Transform Your Assessment Skills: Join Me on March 15! 🤓
Imagine moving beyond textbook knowledge to confident, clinical expertise in neonatal assessment. That's exactly what my live course on March 15 offers!
Whether you're new to the NICU or looking to refine your skills, this interactive session will transform how you approach each neonatal patient—giving you practical techniques and a supportive community of passionate nurses, all focused on mastering neonatal assessment.
📌 Reserve your spot now!
✨ Can't make it live or missed the session? No worries! You'll still have access to the recording.
I look forward to helping you develop the confident, nuanced assessment skills that make exceptional NICU nurses. See you there! 💙👶🏽

Wishing you the best
Amanda 💜
Cardiac Blogs
Neonatal Head to Toe Assessment
Hi there,
I just returned from an amazing conference down in San Diego. I always love learning from the experts about the latest research, QI projects, and ideas to better care for our patients. Do you attend conferences? I think it's a great way to continue developing professionally, staying curious, and learning how we can provide better care for our babies. Let me know if you are planning on attending any upcoming neonatal conferences, maybe I'll see you there!
Neonatal Head-to-Toe Assessment: A Guide for NICU Nurses
When you first hold a newborn patient in your hands as a NICU nurse, every tiny detail matters. Performing a comprehensive neonatal assessment isn't just a clinical task—it's your window into understanding what your patient needs when they can't tell you themselves. This structured approach blends careful observation, precise auscultation, and gentle palpation to reveal crucial clinical information that could make all the difference in a newborn's care journey.

The Art of Silent Assessment: Observation First 👀
Before your hands ever touch the baby, your eyes should be collecting vital information. This initial observation period tells a story:
Watch how the newborn's skin tone appears across their body—is it the healthy pink we hope to see, or are you noticing concerning pallor, plethora, jaundice, or the bluish tint of cyanosis? Notice how the baby moves—are their movements smooth and purposeful, or do you see concerning limpness or jitteriness that suggest neurological or musculoskeletal issues? Pay special attention to their breathing effort—the subtle signs of retractions between the ribs, nostrils flaring with each breath, or the telltale grunting of respiratory distress can alert you to problems before monitors do. Finally, assess their state of alertness—whether peacefully sleeping, quietly observing the world, actively engaged, or crying in distress—as this offers insights into both their neurological status and immediate needs.
Head Assessment 👶
The newborn's head holds many clues about their birth experience and neurological health:
When you palpate the fontanelles and suture lines, you're checking not just for normal development but for signs of increased intracranial pressure or premature fusion. You'll likely encounter common findings like caput succedaneum (swelling that crosses suture lines and typically resolves within days) or cephalohematoma (swelling confined by suture lines and potentially taking weeks to resolve). But remain vigilant for the rare but dangerous subgaleal hemorrhage—a mobile, boggy scalp mass that can rapidly lead to hypovolemic shock and requires immediate intervention.
Skin Assessment 🖐️
A newborn's skin can tell us a lot about their overall health, don't forget the skin is our bodies largest organ:
The creamy vernix protecting a term newborn's skin and the fine lanugo covering a premature baby's body are normal findings that tell you about gestational age. You'll commonly spot benign conditions like erythema toxicum (those harmless white vesicles on red bases that are sometimes referred to as “baby acne”) or tiny white milia cysts across the nose and cheeks. While many birthmarks like Mongolian spots or strawberry hemangiomas are harmless, be alert for concerning signs like petechiae, pustules, or large bruises that might signal infection or bleeding disorders requiring prompt attention.
Cardiovascular System 🫀
The cardiovascular assessment goes far beyond just checking numbers on the monitor:
You should auscultate a heart rate between 100-160 beats per minute in a calm, resting newborn. Listen carefully through all cardiac cycles for murmurs that might suggest structural heart problems. The comparison between brachial and femoral pulses is particularly crucial—diminished or absent femoral pulses could be your first clue of coarctation of the aorta, a condition requiring timely intervention. And don't forget signs of perfusion, like capillary refill... we want to see a brisk refill under 3 seconds.
Respiratory Assessment 🫁
A newborn's breathing pattern reveals volumes about their adaptation to extrauterine life:
While counting those 40-60 breaths per minute, you're watching for the subtle signs of respiratory distress that might indicate the need for support. The fine crackles you hear during the first few hours are often simply the sound of fetal lung fluid clearing—a normal transition phenomenon. However, high-pitched stridor demands attention as it suggests airway obstruction. And if your stethoscope picks up bowel sounds where lung sounds should be, consider the possibility of congenital diaphragmatic hernia (CDH), where abdominal organs have migrated into the chest cavity.‼️
Abdominal Assessment 🍼
The abdomen holds clues about multiple organ systems:
A symmetrical, gently rounded abdomen is what we hope to find, but deviations tell important stories. A scaphoid (sunken) abdomen in conjunction with respiratory distress might suggest CDH, while distention could indicate anything from harmless "CPAP belly" to a concerning intestinal obstruction. Those active bowel sounds should appear within the first hours after birth as the intestines fill with gas.
Genitourinary Assessment 💩
This assessment provides insights about both current function and future development:
For male infants, checking for hypospadias isn't just about noting abnormal urethral placement—it's also critical information for preventing inappropriate circumcision that could complicate future surgical repair. In female infants, the pseudo-menses you might observe is simply the body's response to maternal hormones withdrawal—a normal finding that often alarms new parents. Tracking urinary output in the precise measurements in mL/kg/hr gives you quantifiable data about kidney function and overall fluid balance that guides critical treatment decisions.
Musculoskeletal & Neurological Assessment 🧠
How a newborn moves and responds reveals their neurological integrity:
When you check the clavicles after a difficult delivery, you're looking for the subtle signs of fracture that might explain decreased arm movement. The primitive reflexes—Moro, grasp, stepping, Babinski, Galant..—provide a window into neurological development and function. An asymmetric Moro reflex might be your first indication of brachial plexus injury, while asymmetric gluteal folds could signal developmental dysplasia of the hip that, if caught early, can prevent years of mobility challenges.
Transform Your Assessment Skills: Join Me on March 15! 🤓
Imagine moving beyond textbook knowledge to confident, clinical expertise in neonatal assessment. That's exactly what my live course on March 15 offers!
Whether you're new to the NICU or looking to refine your skills, this interactive session will transform how you approach each neonatal patient—giving you practical techniques and a supportive community of passionate nurses, all focused on mastering neonatal assessment.
📌 Reserve your spot now!
✨ Can't make it live or missed the session? No worries! You'll still have access to the recording.
I look forward to helping you develop the confident, nuanced assessment skills that make exceptional NICU nurses. See you there! 💙👶🏽

Wishing you the best
Amanda 💜
hey nurses don't miss out
© Copyright 2024. AmandasNICUEd. All rights reserved. | Terms & Conditions | Privacy Policy Contact: [email protected]


