
Welcome to Amanda's NICU Education




Hi! My name is Amanda. I'm a NICU nurse, Clinical Nurse Specialist, NICU Educator... basically your NICU BFF. If you want to talk NICU, I'm here for you! I love everything about NICU nursing and I'm eager to learn and share my knowledge with all my NICU friends.
I have been a NICU nurse since 2009 I am currently a Clinical Nurse Specialist in a Level IV NICU in Los Angeles.
I am passionate about educating the next generation of NICU nurses. I share my knowledge through platforms such as Instagram and Facebook and am excited to have you here on my website!
Click on the button below to sign up for my newsletter filled with NICU education and tips for all experience levels.

Not very many people love taking tests but as a self-acclaimed "forever student" who has taken (and passed) five different certification exams I am no longer afraid of tests! "Way to brag", you might be thinking but I want to help YOU pass your certification exam too!
Introducing Amanda's RNC-NIC Success digital course - your ultimate study companion!
Gain unlimited, on-demand access for life, ensuring you're primed to ace your certification exam.
I'm here to help you succeed and I can't wait for you to share with me that you PASSED the RNC-NIC EXAM!!!









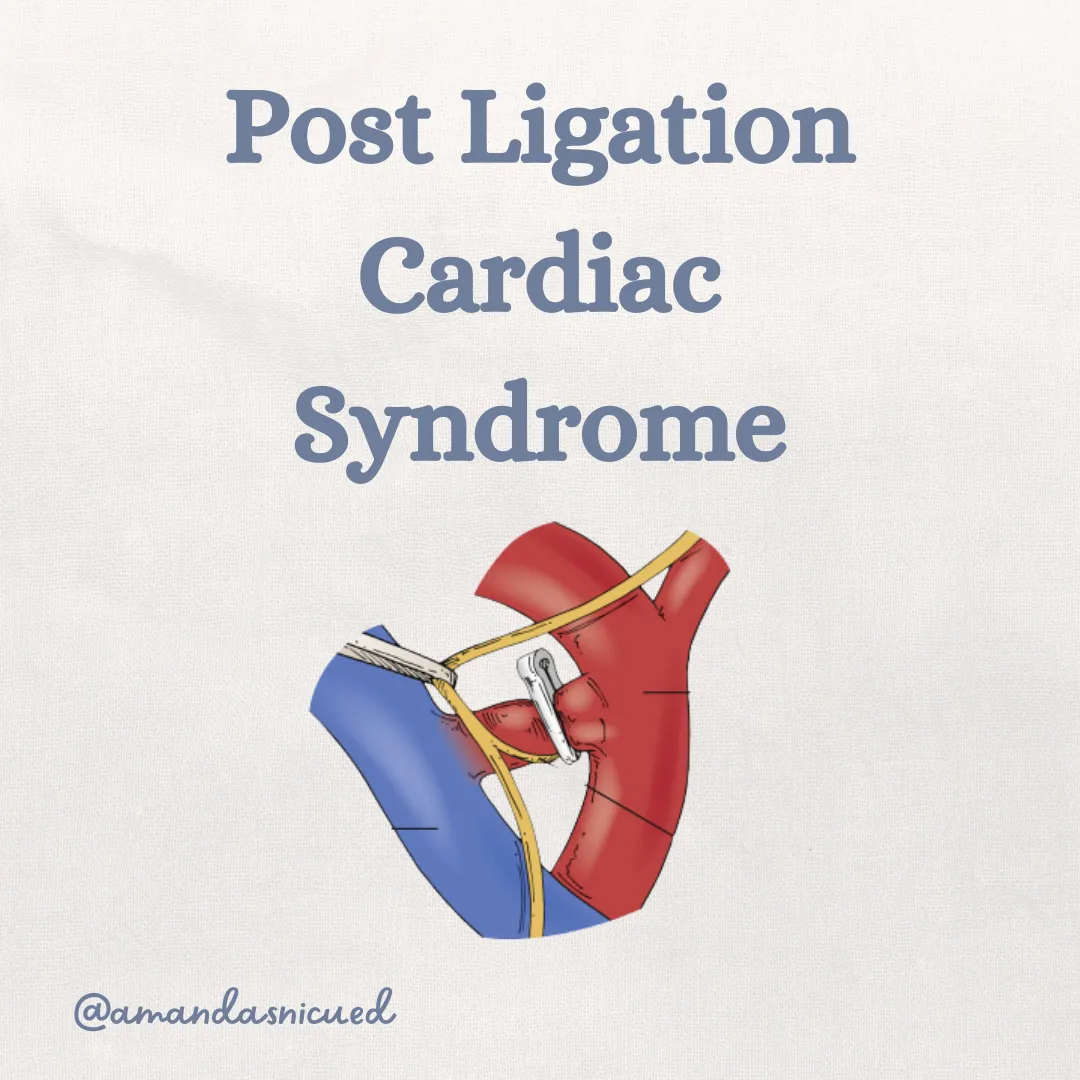
Post Ligation Cardiac Syndrome
A few weeks ago I was talking to a friend at the NeoHeart conference. We were discussing the complication post-ligation cardiac syndrome, when a patient deteriorates after having their patent ductus arteriosus ligated. Have you seen this occur? Let's review together...
Click Here for the RNC-NIC Certification Course
Pathophysiology
Let's refresh our memories on the patterns of blood flow for the fetus, in the newborn after birth with a hemodynamically significant patent ductus arteriosus, and after the ductus is ligated.
In the fetus, recall the ductus arteriosus is one of the necessary fetal shunts allowing blood to flow from the pulmonary artery (PA) to the aorta (AO) (right to left). Normal circulation in the fetus involves oxygenated blood flowing from the umbilical vein, through the ductus venosus, and into the right atrium. The majority of the blood flows directly through the foramen ovale into the left atrium, down to the left ventricle and up the aorta to the brain and other organs and back to the placenta via the umbilical arteries. Deoxygenated blood enters from the superior vena cava (SVC) and inferior vena cava (IVC) and travels into the RA down into the RV, up the PA and across the ductus arteriosus (DA). Remember pulmonary pressures are very high in the fetus and only about 2% of blood flows into the lungs.
RNC-NIC Tip: Remember the three fetal shunts and why they are important to fetal circulation:
Ductus venosus: shunts blood from the umbilical vein into the IVC, bypassing the portal veins.
Foramen ovale: allows shunting between the RA and LA
Ductus Arteriosus: allows shunting between the PA and AO
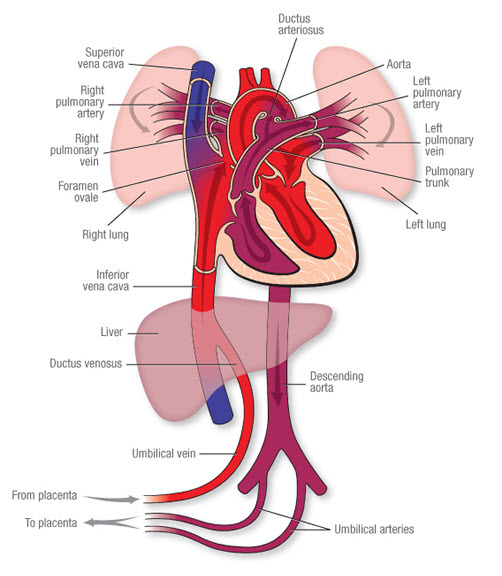
American Heart Association, 2023
Newborn with a Hemodynamically Significant PDA (hsPDA)
After birth, the placenta is gone, systemic vascular resistance (SVR) rises, and pulmonary vascular resistance (PVR) falls as the lungs inflate with air. In most babies, the DA closes naturally within hours to days, but in preterm infants with an hsPDA, the DA stays open. Since the PVR has decreased the flow reverses (remember blood always flows the path of least resistance). Blood moves from the high-pressure AO into the PA (left-to-right shunting). This can overload the lungs with too much blood flow, making gas exchange harder, and “stealing” blood from systemic organs like the kidneys, gut, and brain (aka "diastolic steal"). Over time, the left ventricle has to work harder, leading to dilation and possibly ventricular dysfunction.
Post PDA Ligation
When the ductus arteriosus is surgically tied off or occluded with a device, the hemodynamics change instantly. The pop off for LV output is gone, and the afterload is significantly increased. In some babies especially preterm infants with immature, less compliant hearts this can trigger Post Ligation Cardiac Syndrome (PLCS). This typically develops within 6–12 hours after closure and can involve severe hypotension, reduced cardiac output, signs of poor organ perfusion and increased ventilation and oxygenation requirements.

El-Khuffash, Jain, & McNamara, 2011
What is PLCS?
Post-ligation cardiac syndrome (PLCS) is defined as severe hemodynamic and respiratory collapse within 24 h of PDA closure, requiring initiation or an increase of an inotropic agent by > 20% of preligation dosing and an absolute increase of at least 20% in ventilation parameters compared with the preoperative value.
Why PLCS Happens
Sudden Increase in Afterload: The immature neonatal myocardium isn’t built for large afterload shifts. The muscle fibers are less organized and have limited to no ability to increase stroke volume.
Reduced Preload: Pulmonary venous return can fall after closure, decreasing the amount of blood returning to the left side of the heart.
Immature Cardiac Adaptation: Preterm hearts have lower contractile reserve, making them prone to failure when stressed.
Inflammatory and Stress Response: Surgical handling, anesthesia, and pain can trigger systemic inflammation, worsening myocardial performance.
Surgical Ligation vs Transcatheter Closure
PLCS is more common after surgical ligation.
Why? The sudden removal of the low-resistance PDA shunt can cause abrupt increases in left ventricular afterload, a drop in cardiac output, and systemic hypotension.
In Duboue et al.’s 2024 multicenter study, PLCS rates were significantly lower in transcatheter group compared to surgical ligation, likely because transcatheter closure tends to produce a more gradual change in loading conditions and often occurs in more stable, older infants.

Zaoui, 2023
What Nurses Should Look For at the Bedside
PLCS can be sneaky in its early stages, so your continuous assessments are critical. Here’s what to watch:
Cool Skin & Prolonged Cap Refill: These are classic signs of low cardiac output.
Respiratory Instability: Ventilator settings may need to be increased, or oxygen needs may rise as cardiac output drops.
Urine Output Falls: A drop in urine output, or rising creatinine, means kidneys aren’t being perfused well. Make sure you are frequently calculating urine output.
Blood Gas: A metabolic acidosis may be your first lab clue of poor cardiac output.
ECHO Findings: While you may not be the one doing the echo, knowing that decreased LV function or a low velocity outflow can confirm the diagnosis helps you understand the plan.
Blood Pressure Drops: Hypotension is a hallmark. If MAPs are persistently low and not responding to volume, think PLCS.
Post-surgical patients require vigilant monitoring for hypotension, poor perfusion, metabolic acidosis, and escalating ventilatory needs within the first 12–24 hours.... these are classic PLCS red flags.
Post-TC patients may still develop hemodynamic instability, but it’s less abrupt; watch for arrhythmias, oxygen requirement changes, and femoral site complications.
How We Manage PLCS
Management is all about restoring balance between oxygen delivery and demand.
Early Recognition: In the first 24 hours post-closure, vitals should be trended, not just spot-checked. Watch the patterns (gradual BP drop, increasing FiO₂, or creeping lactate should ring alarm bells).
Hemodynamic Support:
Inotropes like dobutamine or milrinone are used to support contractility and reduce afterload.
Vasopressors like norepinephrine or dopamine may be needed if SVR is too low.
Fluid Optimization: A fluid bolus could be helpful if there is low preload but not every hypotensive baby needs a fluid bolus. Too much fluid can worsen lung congestion.
ECHO-Guided Therapy: Bedside functional echo can help the team choose the right medication mix: whether the heart needs more squeeze, more volume, or reduced afterload.
Key Points for Your Practice
Always assume PLCS could happen: especially after surgical ligation in a sick preterm infant.
Watch the trends: a steady drift in BP, lactate, or urine output can be more telling than a single abnormal reading.
Partner with the medical team: communicate subtle changes early, before instability becomes severe.
Educate families: explain that PDA closure changes how the baby’s heart works, and why close observation is critical for a day or two afterwards.
Missed my other newsletters? Click here to read them!
References:
El-Khuffash, A., Jain, A., & McNamara, P. (2011). Enhancing the Care of Preterm Infants Undergoing Surgical Ligation of a Patent Ductus Arteriosus [Review of Enhancing the Care of Preterm Infants Undergoing Surgical Ligation of a Patent Ductus Arteriosus]. Neonatology Today, 6(8). https://www.neonatologytoday.net/newsletters/nt-aug11.pdf
Silva, I. A., Corso, R. B., Pina, G., Santos, M. V. N., Souza, H. J. B., Fenelon, M. P. M., Alves, L. J. S. R., Vasconcelos, D. L., & Marques, V. B. P. (2022). Post Ligation Cardiac Syndrome: an Educational Presentation. Brazilian journal of cardiovascular surgery, 37(1), 128–130. https://doi.org/10.21470/1678-9741-2020-0278
Duboue, P. M., Padovani, P., Bouteiller, X. P., Martin-Kabore, F., Benbrik, N., Gronier, C. G., Bouissou, A., Garnier, E., Mitanchez, D., Flamant, C., Rozé, J. C., Baruteau, A. E., & Lefort, B. (2024). Post-ligation cardiac syndrome after surgical versus transcatheter closure of patent ductus arteriosus in low body weight premature infants: a multicenter retrospective cohort study. European journal of pediatrics, 183(5), 2193–2201. https://doi.org/10.1007/s00431-024-05481-y
Giesinger, R. E., Bischoff, A. R., & McNamara, P. J. (2019). Anticipatory perioperative management for patent ductus arteriosus surgery: Understanding postligation cardiac syndrome. Congenital heart disease, 14(2), 311–316. https://doi.org/10.1111/chd.12738
Zaoui N, Boukabous A, Irid N, Babou K, Benamara S (2023) Percutaneous Patent Ductus Arteriosus (PDA) closure: When and how to close Coil VS Occluder “step by step” cases report. J Vaccines Immunol 9(1): 015-023. DOI: 10.17352/jvi.000056

December 2023 Certification Review Webinar
NICU Certification Review


Ready to kickstart your journey to becoming a certified NICU nurse?
Look no further!
Grab my FREE E-Book packed with essential study and test-taking strategies for the RNC-NIC.
In the E-Book I give you the resources you need including the link to access the candidate guide, several types of books to study from, some of my favorite strategies, an outline of the content you should review, and a blank calendar for you to make your study plan!
Frequently Asked Questions About the RNC-NIC exam

What is the RNC-NIC?
The RNC-NIC is a competency-based exam that tests the specialty knowledge of nurses in the United States & Canada who care for critically ill newborns and their families.
The RNC-NICU is a nationally recognized certification that recognizes the registered nurse for their specialty knowledge and skill.

Who can take the RNC-NIC exam?
Nurses can take this exam after a minimum of two years experience in the NICU caring for critically ill newborns and their families.

Which books should I use?
I'm glad you asked! There are many excellent books to help you prepare for the RNC-NIC, I gathered ande describe each of them for you in my FREE e-book.
Is there a course to help me study?
Yes! Many hospitals host their own certification course and there are a few online courses. See my RNC-NIC test taking tips E Book for more information
What happens if I don't pass the exam?
If you don't pass the exam on your first try you can try again after 90 days. You will have to reapply after 90 days and pay a retest fee. There is no limit to the number of times you can take the exam (however a candidate can only sit for the exam twice per year).

Can I make more money if I take the RNC-NIC exam and get certified?
Yes! Many hospitals provide a raise or a bonus for nurses with specialty certifications. Hospitals also typically hire at a higher base salary when nurses have a certification.

Find me @amandasnicued on these channels or Email me
hey nurses don't miss out
© Copyright 2024. AmandasNICUEd. All rights reserved. | Terms & Conditions | Privacy Policy Contact: [email protected]

